MedComm | Bone marrow mesenchymal stem cell-conditioned medium facilitates fluid resolution via miR-214-activating epithelial sodium channels

Open the phone and scan
Acute lung injury (ALI) is featured with severe lung edema at the early exudative phase, resulting from the imbalance of alveolar fluid turnover and clearance. Mesenchymal stem cells (MSCs) belong to multipotent stem cells, which have shown potential therapeutic effects during ALI. Most precious studies focused on the inflammation moderation, tracking to impaired tissues, and the attenuation of lung permeability by MSCs in ALI therapy, whereas the mechanisms of MSC-CM in restoring lung edema, especially how MSC-CM modulated the ENaC-related fluid transport in alveolar epithelium was rarely reported. MSCs have the ability to regulate the immune response to tissue damage and promote repair in vivo, and have been suggested to act on a variety of lung diseases (including ALI). Of note, MSCs can release lots of cytokines/growth factors, signal lipids, exosomes, and miRNAs. By performing microarray hybridization, Chen et al found at least 151 miRNAs in MSC through testing the RNAs. The authors also have previously tested several miRNAs, including miR-124-5p, miR-130b, and so on, and found that the miR-124-5p participated in the regulation of MSC-CM in lipopolysaccharide (LPS)-induced ALI by targeting α-ENaC.

Similarly, miR-214 was found in MSCs and has been reported to exert key roles in various inflammatory diseases, whereas its role in ALI and the relative mechanisms are seldom studied. Therefore, the authors chose miR-214 as their main research object, and cultured it with alveolar type 2 epithelial (AT2) cells to explore its role in the regulation of MSC-CM in LPS-induced ALI, aiming to provide a novel direction for therapeutic strategy in ALI. In this study, AFC was increased significantly by intratracheally administrated MSC-CM in lipopolysaccharide-treated mice. MSC-CM augmented amiloridesensitive currents in intact H441 monolayers, and increased α-epithelial sodium channel (α-ENaC) expression level in H441 and mouse alveolar type 2 epithelial cells. Meanwhile, MSC-CM increased the expression of miR-214, which may participate in regulating ENaC expression and function. The results suggested that MSC-CM enhanced AFC in ALI mice in vivo through a novel mechanism, involving miR-214 regulation of ENaC (Fig. 1).
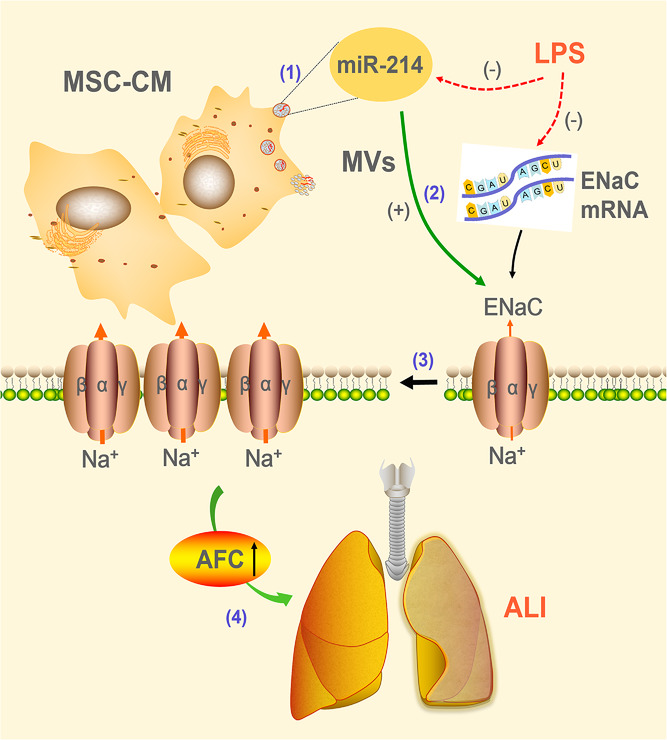
Fig.1 Potential mechanisms for MSC-CM to rescue LPS induced lung epithelial injury


